Imagine your body is a house protected by a high-tech security system.
Usually, this system—your immune system—is amazing. It spots burglars (like viruses) and chases them away to keep you safe.
But for millions of people, the security system glitches. Instead of looking for intruders, it gets confused. It starts attacking the furniture, the walls, and the windows. It treats your own healthy cells like the enemy.
This is what it means to live with an autoimmune disease.
If you’re dealing with this, you aren’t alone. You’re part of a massive club. Recent studies estimate that over 15 to 20 million Americans live with an autoimmune condition. That’s roughly 1 in 20 people.
Whether you’re managing Lupus, Rheumatoid Arthritis (RA), or Hashimoto’s, you know the drill. Some days are easy. Other days, you wake up feeling like you’ve been hit by a truck.
These bad days are called an autoimmune flare.
The good news? You aren’t helpless. While you should always work with a doctor, the data shows that specific lifestyle changes—like an anti-inflammatory diet—can help “calm the storm” inside your body. Here is how to navigate an autoimmune flare without losing hope.
What Is an Autoimmune Disease? (The Glitch)
To manage your health, you have to know the players. There are more than 80 known autoimmune diseases, but here are three of the most common ones:
- Rheumatoid Arthritis (RA): This isn’t just “creaky knees.” The immune system attacks the lining of your joints, causing heat, swelling, and pain.
- Lupus (SLE): Think of this one as a shapeshifter. It can target almost anything—your skin, joints, kidneys, or even your brain.
- Hashimoto’s Thyroiditis: Here, the target is the thyroid gland in your neck. Since the thyroid controls your metabolism, attacks can make you feel exhausted, cold, and prone to weight gain.
Recognizing the Signs of an Autoimmune Flare
These conditions are chronic, meaning they don’t just go away. But they do come in waves.
An autoimmune flare is when that wave crashes down. You might feel fine on Tuesday, but on Wednesday, you can barely get out of bed. It is a sudden, sharp increase in symptom severity.
Why does an autoimmune flare happen? According to the Mayo Clinic, triggers vary by person, but the usual suspects are stress, infections, too much sun (especially for Lupus), and inflammatory foods.
5 Lifestyle Tips to Manage an Autoimmune Flare
Medicine is vital, but your daily habits are the foundation. Think of these tips as tools to help you weather the storm when an autoimmune flare strikes.
1. Put Out the Fire (The Anti-Inflammatory Diet)
Think of inflammation like a small fire inside your body. When you’re flaring, that fire grows. Your goal with food is to throw water on it, not gasoline.
Does food really matter during an autoimmune flare? Yes.
Large clinical trials have shown that nutrients play a huge role. For example, studies found that taking Vitamin D and Omega-3 supplements daily reduced the risk of developing autoimmune issues by roughly 22% to 30% over five years.
The “Water” Foods:
- Omega-3s: Fatty fish like salmon and tuna are superstars.
- Color: If it’s bright (berries, leafy greens, sweet potatoes), eat it. These antioxidants help repair cells.
- Spice: Turmeric and ginger are natural painkillers.
The “Gasoline” Foods:
Processed sugar and fried foods fan the flames. Many people find that avoiding gluten or dairy helps reduce the severity of an autoimmune flare.
2. The Spoon Theory (Mastering Your Energy)
When you are navigating an autoimmune flare, you have a limited energy budget. There’s a famous metaphor for this called the “Spoon Theory.”
Imagine you start the day with 12 spoons. Getting dressed costs one spoon. A stressful meeting costs four. Cooking dinner costs two. If you use all your spoons by 5:00 PM, you’re done. You have nothing left to give.
During a flare, you might wake up with only 6 spoons.
- Respect the limit. If you’re out of spoons, rest. Pushing through the pain usually just makes the autoimmune flare last longer.
- Prioritize ruthlessly. Do the one most important thing today. Let the laundry wait.
3. Stress Management Is Medicine
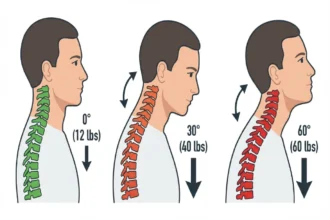
We often think stress is just “in our heads.” But stress produces a hormone called cortisol. While cortisol helps in short bursts, chronic stress confuses your immune system even more, potentially triggering an autoimmune flare.
This isn’t just “feel-good” advice. Research on chronic illness shows that mind-body practices—like mindfulness or gentle yoga—can reduce pain and anxiety scores by 20% to 30%.
Try this:
Take slow, deep breaths for just two minutes. It signals your nervous system that you are safe, allowing your body to switch from “defense mode” to “repair mode.”
4. Prioritize Deep Sleep for Repair
Sleep is when your body goes into the shop for repairs. It is critical for shortening an autoimmune flare.
Data shows that poor sleep is directly linked to higher levels of inflammation. If you cut your sleep short, you’re basically turning up the volume on your pain.
- The Strategy: If you’re flaring, you might need more than 8 hours. Don’t feel guilty about napping. It’s productive time for your cells.
5. Be Your Own Detective (Tracking Triggers)
You are the expert on your body. Keep a simple note in your phone tracking:
- What you ate.
- How you slept.
- How much pain you’re in.
Over time, you’ll spot patterns. You might realize, “Oh, every time I have a stressful week and eat pizza, I get an autoimmune flare the next day.” That knowledge is power.
Medical Support for Autoimmune Flares
Lifestyle changes are amazing, but they work with medicine, not instead of it.
Diagnosing these conditions can be tricky—it’s often a puzzle involving symptoms and blood tests (like the ANA test) to look for those confused immune cells. Doctors use medications like corticosteroids or biologics to calm the immune system down so it stops attacking you.
Don’t be afraid to use them to manage a severe autoimmune flare. They are there to protect your organs from long-term damage.
FAQs
What triggers an autoimmune flare-up?
Common triggers for an autoimmune flare include high levels of emotional stress, physical infections (like the flu), poor sleep quality, and dietary choices such as processed sugars or gluten. Environmental factors, particularly UV sunlight exposure in Lupus patients, are also frequent catalysts for a sudden increase in symptoms.
What is the best diet for autoimmune disease?
An anti-inflammatory diet is most effective. Focus on whole foods rich in Omega-3 fatty acids (like salmon and walnuts), antioxidants from colorful fruits and vegetables, and spices like turmeric. Many patients also find relief by eliminating inflammatory triggers such as processed foods, added sugars, gluten, and dairy.
How can I stop an autoimmune flare naturally?
While medical treatment is often necessary, you can manage severity by “pacing” your energy (resting before you are exhausted), prioritizing 8+ hours of sleep, and practicing stress-reduction techniques like deep breathing. Supplements like Vitamin D and Omega-3s have also been shown to help regulate the immune response.
What is the Spoon Theory for chronic illness?
The “Spoon Theory” is a metaphor used to explain the limited energy reserves of people with autoimmune conditions. It visualizes daily energy as a set number of “spoons.” Every task, from showering to working, costs a spoon. Once the spoons are gone, the person has no energy left and must rest.
The Bottom Line
Having an autoimmune disease can feel incredibly unfair. It’s frustrating to feel like your body is working against you, especially when you “look fine” on the outside.
But you have more control than you think.
By fueling your body with the right food, respecting your energy limits, and giving yourself permission to rest, you can reduce the frequency of every autoimmune flare. You can take the wheel back from your immune system.
Be patient with yourself. You’re doing the best you can with a body that’s fighting a hard battle.
Disclaimer: This blog post is for informational purposes only and does not constitute medical advice. Always consult with your doctor or rheumatologist for diagnosis and treatment suited to your specific needs.