It starts with a headache that won’t go away, no matter how much water you drink. Or maybe it’s a knot in your stomach every Sunday night. Or chronic back pain that flares up whenever you visit your parents, even though you didn’t lift a single heavy box.
You go to the doctor. They run blood tests. They scan your spine. Then, they give you the answer that feels like a dismissal: “Everything looks normal. It’s probably just stress.”
But it doesn’t feel “just” like anything. It feels real.
If you are dealing with unexplained pain, you might be experiencing the physical symptoms of trauma. This is the physical echo of your past, appearing in the present.
For a long time, we treated mental health and physical health like they were divorced—the mind went to the therapist, and the body went to the doctor. But modern science has proven that this separation is an illusion. Your body and your biography are tied together.
Here is why trauma stored in the body might be causing your pain, and how you can gently teach your system to let go.
What Are the Physical Symptoms of Trauma?
First, let’s clear up a misconception. When we hear the word “trauma,” we usually think of catastrophic events like war or a car crash. Psychologists call these “Big T” traumas.
But there is also “Little t” trauma. These are the quiet, ongoing stressors: growing up in a chaotic home, feeling constantly criticized, emotional neglect, or financial instability.
According to mental health experts, trauma isn’t just about the event itself. It’s about how your nervous system processed it. If you went through something where you felt unsafe or helpless—and you didn’t have the support to work through those feelings—your brain may have hit the “Record” button, but it never hit “Stop.”
As a result, the physical symptoms of trauma can manifest years later as:
- Chronic fatigue or exhaustion
- Unexplained muscle tension
- Digestive issues (IBS)
- Sleep disturbances
- autoimmune flare-ups
The Science: Why Trauma Stored in the Body Causes Pain
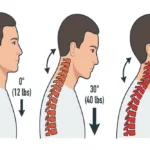
To understand why your back hurts when you’re anxious, we have to look at the brain.
Imagine your amygdala (the danger-sensing part of your brain) is a smoke detector. In a healthy system, the alarm blasts when there is a fire, and shuts off when you’re safe.
But for survivors of emotional trauma, that smoke detector gets recalibrated. It becomes incredibly sensitive. It starts going off when you burn toast. It screams when someone raises their voice, or when you smell a certain cologne.
When this alarm rings, your body floods with cortisol. Your muscles tense up to fight. Your digestion shuts down to save energy. When this state becomes chronic, it creates the physical symptoms of trauma we often mistake for random illness.
The “Phantom” Pain (Central Sensitization)
This constant state of high alert leads to something called central sensitization. Essentially, the volume knob on your pain receptors gets stuck on “High.”
This explains why so many people with trauma histories deal with things like fibromyalgia, IBS, or chronic pain. The hardware is fine, but the software is glitching.
A Real-Life Example:
Take “David,” a 40-year-old accountant. He had severe stomach issues for years that no diet could fix. In therapy, David realized his stomach pain mimicked the feeling he had as a kid when his unpredictable father came home.
Thirty years later, David is safe. But whenever his boss walks by, his stomach clenches. His nervous system is time-traveling back to 1995, recreating the physical symptoms of trauma daily.
The Stats: Adverse Childhood Experiences (ACEs) and Health
If you’re wondering, “Is this just me?”, the answer is a hard no.
This connection is backed by the famous Adverse Childhood Experiences (ACE) study. Researchers found that childhood stress is a massive predictor of adult health and the development of physical symptoms of trauma.
- It’s common: About 64% of adults have at least one of these experiences.
- It adds up: About 16% report four or more ACEs.
- The impact is real: People with higher ACE scores (4+) were found to be 2 to 3 times more likely to deal with heart disease or depression later in life.
But here is the most important part:
Risk is not destiny.
Think of it like having high cholesterol. It means you have a higher risk factor, yes. But it doesn’t guarantee you will get sick. It just means you need to take special care of your nervous system. Many people with difficult pasts reverse the physical symptoms of trauma because they find the right tools to heal.
3 Strategies to Heal Physical Symptoms of Trauma
If this feels heavy, take a deep breath. You aren’t broken. Your body did exactly what it was designed to do: it adapted to survive a hard environment.
Now, the goal is to tell your body that the war is over. You can’t just “think” your way out of physical symptoms of trauma; you have to show the body it’s safe.
1. Practice “Interoception” (The Safety Check)
Trauma makes us live in our heads because the body feels unsafe. We need to slowly reconnect.
- The Strategy: Set a timer for one minute. Close your eyes. Can you feel your feet on the floor? Can you feel your shirt against your arm?
- Why it works: You’re training your brain to notice physical sensations without panicking. You’re teaching the amygdala, “See? We are in our body, and we are safe.” This simple act can reduce the intensity of physical symptoms of trauma over time.
2. Complete the Stress Cycle
Ever see a dog shake itself off after a fight with another dog? They are physically releasing the stress energy. Humans tend to sit still and stew in it, which locks trauma stored in the body into your muscles.
- The Strategy: When you feel triggered or stressed, move. Shake your hands out vigorously. Do ten jumping jacks. Let out a long, loud sigh.
- Why it works: It signals to your nervous system that the threat is gone and you can return to baseline.
3. Use CBT to Reframe Body Sensations
When pain flares up, the trauma brain whispers, “This will never end. I’m damaged.” This thought often worsens the physical symptoms of trauma by adding anxiety to the pain.
- The Strategy: Catch that thought. Tell yourself, “My chest is tight because I just had a hard conversation. This is a memory of stress, not a heart attack. I am safe in my living room.”
- Why it works: You are using logic to soothe the panicked part of your brain, like a parent calming a scared child.
You Can Heal
Healing from the past isn’t just about talking through memories. It’s about convincing your cells that they are safe now.
If you have been blaming yourself for being “oversensitive” or “sickly,” please stop. Your body has been working overtime to protect you. It has been carrying the load so you could survive.
Recognizing the physical symptoms of trauma is the first step. Now, you can thank your body, and slowly, gently, teach it to put the burden down.
When to Seek Professional Help
While self-regulation helps, physical symptoms of trauma can be stubborn. Therapies like EMDR (which helps process memories) or Somatic Experiencing (which focuses on body tension) can be game-changers.
If the pain is chronic, or if you feel overwhelmed by memories, please reach out to a trauma-informed therapist. You do not have to carry this alone.
FAQs
What are the physical symptoms of trauma?
Physical symptoms of trauma often include chronic fatigue, unexplained muscle tension, sleep disturbances, digestive issues (like IBS), and headaches. These symptoms occur when the nervous system remains in a prolonged state of “fight or flight,” causing the body to manifest emotional distress as physical pain or dysfunction.
Can emotional trauma cause chronic pain?
Yes, emotional trauma can lead to chronic pain through a process called central sensitization. This occurs when the nervous system becomes hypersensitive, amplifying pain signals. This often results in conditions like fibromyalgia, back pain, or migraines, even when medical tests show no structural damage to the body.
How do you release trauma stored in the body?
To release trauma from the body, focus on “bottom-up” processing. Effective strategies include “completing the stress cycle” through physical movement (shaking, dancing, exercise), practicing interoception (mindful body awareness), and utilizing professional therapies like EMDR or Somatic Experiencing to retrain the nervous system’s response to danger.
Does childhood trauma affect adult health?
According to the Adverse Childhood Experiences (ACE) study, childhood trauma is strongly linked to adult health issues. Adults with high ACE scores have a significantly increased risk of developing heart disease, autoimmune disorders, depression, and chronic pain later in life due to the cumulative effect of toxic stress.
Disclaimer: The information provided in this blog post regarding the physical symptoms of trauma is for educational and informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified mental health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.